Ectopic pregnancy is a complication that poses a serious threat to the health and even life of the mother. When ectopic pregnancy the fertilized egg is implanted not in the uterus, but, most often, in the fallopian tube, and the embryo begins to develop. 3-4 weeks after attachment of the fetal egg reaches a critical size and a tube rupture may occur, complicated by massive bleeding. In this case, the clock may count and the woman needs emergency help. That is why it is important to know the symptoms of this threatening condition.
Symptoms of ectopic pregnancy
Ectopic pregnancy on early stages outwardly it can manifest itself with classic symptoms - delayed menstruation, toxicosis, weakness, sensitivity in the chest. However, there are a number of symptoms that can tell a woman that all is not well with her health. First of all, these are pressing and bursting pains in one side or throughout the entire abdominal cavity (depending on the place of attachment of the embryo), as well as scanty bleeding. These symptoms require urgent medical attention.
Another symptom of an ectopic pregnancy is a slow increase in human chorionic gonadotropin, a hormone secreted by the body during pregnancy. In a normally developing pregnancy, it doubles every 48 hours in the first few weeks. With an ectopic or non-developing pregnancy, it grows more slowly or does not grow at all.
Rectal temperature during ectopic pregnancy
A complication can also be suspected based on additional signs. Indicators of basal temperature during pregnancy that develops normally and during ectopic pregnancy differ. During pregnancy, the temperature rises sharply immediately after ovulation and remains consistently high (above 37°C). The temperature during an ectopic pregnancy can jump up and down, the picture looks blurry, and the graph may drop. If you are experiencing a delay, but the temperature chart is not typical for a normal pregnancy, you should also consult a doctor. Body temperature during an ectopic pregnancy can also be elevated due to, for example, the onset of inflammation or the action of hormones.
Only a doctor can reliably determine the presence of an ectopic pregnancy based on the totality of symptoms and an ultrasound scan. However, knowing the answer to the question - what the temperature may be during an ectopic pregnancy, as well as what symptoms may accompany this condition, you can quickly consult a doctor and save your health and life.
By nature, women strive for motherhood and therefore, in preparation for it, they try to learn as much as possible about the peculiarities of pregnancy and childbirth. And probably many of them have heard of such a thing as basal temperature. In this regard, women often wonder how the temperature behaves during an ectopic pregnancy and whether it differs from the basal temperature during uterine implantation of the egg.
How does basal temperature change in women?
Hormonal levels during the period menstrual cycle women have different ones. In the first phase, the hormone estrogen predominates, and in the second, progesterone. Progesterone enhances metabolism in a woman’s body and helps increase basal temperature above 37 degrees (usually 37.1-37.2 degrees Celsius). This temperature lasts until the onset of menstruation and then decreases. If pregnancy occurs, basal temperature remains elevated.
In the early stages of pregnancy, measuring basal temperature is important for diagnosing certain abnormalities. Sometimes an increase or decrease in basal temperature indicates a hormonal imbalance in a woman’s body and suggests a threat to the normal course of pregnancy. Therefore, many women, for example, are interested in the question of what the temperature is during an ectopic pregnancy.
There is no need to measure basal temperature for all women without exception and throughout pregnancy. Gynecologists advise it to be measured by those pregnant women who, unfortunately, have already experienced an ectopic pregnancy, cessation of fetal development, miscarriage and other complications.
Basal temperature during ectopic pregnancy
Some women believe that basal temperature does not increase during an ectopic pregnancy. This is incorrect - progesterone in this case is produced in the same way as during normal pregnancy, which leads to an increase in temperature. Therefore, during both normal and ectopic pregnancy, the basal temperature is usually above 37 degrees Celsius.
Sometimes you can observe a decrease in basal temperature during an ectopic pregnancy below 37 degrees Celsius. Based on this, it can be assumed that the development of the embryo has stopped. This condition is called frozen pregnancy. It can be observed in both intrauterine and ectopic pregnancies. In these cases, the corpus luteum stops performing its functions as an endocrine gland and undergoes regression, so the level of progesterone in the woman’s blood sharply decreases and, as a result, the basal temperature decreases during an ectopic pregnancy.
An ectopic pregnancy does not always lead to tube rupture and massive internal bleeding. Often it is interrupted as a tubal abortion. In this case, the fertilized egg dies, it peels off from the wall of the fallopian tube and is expelled into the abdominal cavity.  The bleeding in this case is not as pronounced as when a pipe ruptures. However, blood accumulating in the abdominal cavity contributes to the development of the inflammatory process, which is manifested by malaise and pain. In this case, the basal temperature during an ectopic pregnancy increases significantly and can reach 38 degrees.
The bleeding in this case is not as pronounced as when a pipe ruptures. However, blood accumulating in the abdominal cavity contributes to the development of the inflammatory process, which is manifested by malaise and pain. In this case, the basal temperature during an ectopic pregnancy increases significantly and can reach 38 degrees.
Diagnostic reliability of basal temperature during ectopic pregnancy
As we have already found out, the temperature during an ectopic pregnancy can be either increased or decreased. Therefore, based solely on measuring basal temperature, the diagnosis of ectopic pregnancy can neither be confirmed nor rejected. In addition, basal temperature indicators depend on many factors (duration of sleep, physical activity, sex the day before, certain medications, and much more).
If you are tormented by doubts or are worried about pain, bleeding, or general malaise, then you should consult a doctor for the necessary examination. Currently, there are special tests that allow one to suspect an ectopic pregnancy at a very early stage. However, a definitive diagnosis can only be made by ultrasound.
A pregnancy is called ectopic when a fertilized egg implants in the fallopian tube, ovary, abdomen, or cervix. In this case, it is impossible to carry and give birth to a child; in addition, the pathology poses a danger to the health and life of the woman herself. Therefore, it is important to detect symptoms of ectopic pregnancy, diagnose and treat them as early as possible.
The severity of symptoms may vary. Sometimes women already identify the manifestations of pathology in their early stages. But there are situations when ectopic implantation of the fertilized egg becomes known after a sharp deterioration in health and an ambulance is called.
But there are several signs that may indicate ectopic implantation of the embryo:
- Often the test works later than in a normal pregnancy. This is due to the fact that the concentration of hCG increases slowly. If the embryo is located ectopically, the timing of diagnosis is shifted by 2-3 days compared to normal.
- After the first day of delay, the second test strip appears. This is also explained by the slow rise in hCG levels in the urine.
If a specialist suspects the development of an ectopic pregnancy, the following studies are prescribed:
- Laboratory blood test for hCG
. Human chorionic gonadotropin increases more dynamically in the blood than in the urine. Therefore, pregnancy can be confirmed in this way at an earlier date: 5-6 days after fertilization. To find out whether it is ectopic, it is necessary to compare data from several studies. During normal pregnancy, the level of hCG doubles every 2 days; in pathological pregnancy, the changes are insignificant.
- Transvaginal ultrasound
. Using ultrasound, the position of the embryo can sometimes be determined from the 3rd week of pregnancy, but most often it is detected only by 4-5. If the doctor suspects an ectopic pregnancy, but the fertilized egg is not visible (its size is extremely small), then a repeat examination is prescribed or the woman is hospitalized so that she is under constant medical supervision. Transvaginal ultrasound is the most reliable method for diagnosing ectopic pregnancy, but in 10% of cases it also gives an error: the fertilized egg is considered as a blood or fluid clot. Therefore, the examination is always carried out in combination with a blood test for hCG.
-
. The procedure is carried out as a diagnostic procedure only according to indications: when there is a serious suspicion of an ectopic pregnancy (symptoms, hCG dynamics), but it cannot be confirmed using ultrasound. Laparoscopic surgery is performed under anesthesia; small punctures are made using special instruments, where a tube with a camera and light is inserted, and the doctor examines the organs through an image on a monitor. If an ectopic pregnancy is detected, then therapeutic measures are immediately taken (removal of the fertilized egg, etc.).

Symptoms
Since ectopic pregnancy occurs in different ways, specific symptoms may appear gradually, late or completely absent until an emergency condition develops (with bleeding, rupture of the fallopian tube, etc.). Therefore, you should not hope only for a deterioration in your health; it is necessary to carry out diagnostic procedures in parallel: determination of hCG, ultrasound.
The first symptoms of an ectopic pregnancy coincide with those of a normal pregnancy: general weakness, drowsiness appears, and the mammary glands swell. Pathological implantation does not manifest itself in any way at first. A woman may also experience: nausea, vomiting, dizziness.
At this stage, an ectopic pregnancy can sometimes be determined by testing the level of hCG in the urine. As noted above, in this case, its results may be delayed for several days, since the hormone is produced more slowly than usual. Therefore, if a woman notices signs of pregnancy, but the test gives a negative result, it is likely that the fertilized egg has settled outside the uterus.
An ectopic pregnancy in the early stages has the same symptoms as a normal one, but their nature is somewhat different:
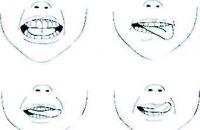
-
. Symptoms of an ectopic pregnancy before a missed period are spotting or slight bleeding. When the embryo is implanted into the wall of the uterus, they are short-lived, lasting several hours. But if it is established outside of it, this symptom will be more intense and lasting.
-
. Often such sensations occur in the lower abdomen. During normal pregnancy, they are tugging and develop due to increased tone of the uterus. With ectopic, they accompany the process of implantation and development of the embryo and can be localized in different areas - where the fertilized egg is attached. Later the pain spreads to the entire abdomen. Its intensity constantly increases - from barely noticeable at first, to sharp, cramping after a few days.
- General malaise
. Normal pregnancy in the early stages may be accompanied by decreased performance, increased drowsiness, and fatigue. With an ectopic, all these symptoms are more pronounced, in addition, dizziness and fainting develop.
- Toxicosis
. Nausea and vomiting often accompany normal pregnancy. At pathological condition these manifestations are more pronounced and intensify every day.
At later stages, the symptoms of ectopic pregnancy increase faster, and in a critical situation - rapidly. A woman’s blood pressure drops sharply, she experiences frequent dizziness, and her body temperature rises. Sometimes there are signs of anemia due to decreased hemoglobin levels.
If the fallopian tube ruptures and internal bleeding develops, this is manifested by very severe pain, shock, and loss of consciousness. Urgent medical attention is required.

For each type of pathological fixation of the ovum, there are characteristic symptoms:
- Pipe
An ectopic pregnancy is manifested by pain on the left or right side, depending on where the implantation of the fertilized egg occurred. If it is fixed in the wide ampulla part, then the symptom appears at 8 weeks, if in the narrow part (in the isthmus) - then at 5-6. The pain intensifies while walking, turning the body, and sudden movements.
- Ovarian
An ectopic pregnancy does not show any pathological symptoms for a long time. This is explained by the fact that the follicle can stretch to fit the size of the embryo. But when the limit of elasticity is reached, severe point pain appears in the lower abdomen, gradually spreading to the lower back and large intestine area. Defecation becomes painful. The attack lasts from several minutes to hours and is accompanied by dizziness and faintness.
- Cervical and cervical-isthmus
ectopic pregnancy occurs without pain. Bloody discharge comes to the fore - from spotting to copious, profuse, posing a threat to life. Due to the increase in the size of the cervix, urination disorders develop (for example, frequent urge).
- Ectopic pregnancy in the abdominal cavity
in the early stages it has symptoms that are no different from those during normal pregnancy. But as the embryo grows, dysfunctions of the gastrointestinal tract appear (constipation, diarrhea, nausea, vomiting), signs of an “acute abdomen” (severe pain, bloating, fainting).
What is an ectopic pregnancy and what symptoms are typical for it? With this pathology, the fertilized egg is implanted outside the uterus: most often in the fallopian tube, less often in the ovary, abdominal cavity, and cervical region.
An ectopic pregnancy can be detected from 4-6 weeks using a blood test for hCG and ultrasound. Symptoms in the early stages are almost the same as during normal pregnancy, but gradually they become more pronounced and specific (localization and intensity of pain, bleeding, disturbances in the functioning of other organs).
Useful video about the symptoms of ectopic pregnancy
Ectopic pregnancy is the second most common cause of death in pregnant women. I think this is a compelling argument not to delay registration when signs of pregnancy appear. Expectant tactics here also threaten the loss of the ability to become pregnant again. Our article will help you recognize the “enemy in person.”
Concept and localization of ectopic pregnancy
An ectopic pregnancy is a pregnancy in which the egg was fertilized, but was finally implanted in a place other than the uterus. It is pathological in that the growing fertilized egg stretches and tears the place of the fetal receptacle, and the chorionic villi destroy the tissues and blood vessels of the attachment site.
Depending on where it was implanted or the location of the fertilized egg - zygote, ectopic pregnancy is given its name:
- pipe The egg, maturing in the ovary, enters the fallopian tube and is fertilized there by a sperm. And then it attaches to the wall of the tube and begins to grow, tearing it apart as the fertilized egg grows. Tubal pregnancy can be: isthmic - when developing in the isthmus of the fallopian tube, ampullary - in the widest section of the tube, fimbrial - in the villi at the exit from the tube, interstitial - at the junction of the tube and uterus;

Since there are no normal conditions for embryo development outside the uterus, chorionic villi penetrate into the tissue of the organ and damage it, causing bleeding into the abdominal cavity
- ovarian - can develop on the surface of the ovary or inside the ovulated follicle. Quite a rare species, occurring in 0.2 to 1.3% of cases;
- abdominal or abdominal - with a probability of occurrence from 0.1 to 1.4% of all cases. When the fertilized egg develops initially in the abdominal cavity - the primary form or gets there after a tubal abortion - the secondary form. In this case, the fertilized egg first secured itself in the fallopian tube, grew so much in 4–8 weeks that the tube ruptured, and from there it entered the abdominal region, but did not die, but settled there and continued to develop;

If the fertilized egg gets into the abdominal region due to a rupture of the tube, then it can become fixed there in the spleen, liver, perimeter (outer layer of the uterus), omentum, intestinal flexures or pouch of Douglas (between the uterus and rectum)
- in the rudimentary uterine horn - a pathology similar to duplication, division of the uterine cavity into two parts, occurs in 0.1–0.9% of cases of all ectopic pregnancies. In this case, one tube and ovary are connected to the uterine cavity, and the second pair of tube and ovary are connected only to the horn, separated by a muscular septum from the uterine cavity;

You can suspect the presence of a rudimentary horn that does not communicate with the uterus by a sharp deterioration in the condition during menstruation - dysmenorrhea: “cotton legs”, vomiting, bloating, severe pain in the lower abdomen, even fainting, increased temperature
- heterotopic pregnancy, in which there are two fertilized eggs, one of them is located in the uterus, and the other is outside it. This is an option for the development of intrauterine and ectopic pregnancies at the same time, the most possible after IVF fertilization in multiple pregnancies (with a probability of 1:00 to 1:30,0000 cases);
- cervical - the zygote was unable to gain a foothold in the uterus due to the characteristics of the tissue lining it and slid down to the narrowed area of the transition to the vagina. The probability of such a situation occurring is from 0.1 to 0.4% of cases;

The danger of this pathology is that there are no signs characteristic of an ectopic pregnancy, and this condition is often confused with the lower insertion of the child’s place
- intraligamentous or intraligamentous - in 0.1% of all cases (or 1 case in 300 cases of ectopic pregnancy) develops in the thickness of the broad ligaments of the uterus, often secondary to a rupture of the fallopian tube towards the mesentery, also possible with a fistula connecting the uterus and tissue around the cervix - parametrium. In this case, it can become attached to the bladder, uterus or pelvic walls;

- combined multiple pregnancy. It is distinguished by a large number of possible combinations of places for fixation of 2.3 fertilized eggs at the same time. The most common combinations are: ampullary + isthmic tubal twin pregnancy or ovarian + interstitial tubal + abdominal triple pregnancy. Due to the widespread use of IVF technologies, the probability of such a pathology is from 1 case in 100 to 1 case in 620 ectopic forms of pregnancy.
In order to assess the likelihood of such a pregnancy occurring in a particular woman, it is better to familiarize yourself with this list of risk groups and consistently mentally cross out the items if they are not relevant to you:

Since I myself, with a bicornuate uterus and frequent inflammations in the vagina, was at risk of developing an ectopic pregnancy, a wave of panic covered me with any delay. I dropped everything and rushed to the ultrasound room. The gynecologist found me good contraceptives and treated me for inflammatory diseases. On her advice, every six months, before each visit to the gynecologist, I undergo foliculometry to be sure of the proper functioning of the reproductive system.
Video: doctor S. Agapkin on predisposing factors that increase the risk of developing an ectopic pregnancy
Causes of ectopic pregnancy
In addition to risk groups, predisposing conditions for the development of ectopic pregnancy include:
Symptoms of ectopic pregnancy
An early ectopic pregnancy does not always manifest itself with clinical symptoms or may not differ in any way from the symptoms of a normal intrauterine pregnancy in the form of breast swelling, vomiting, increased fatigue and drowsiness.
Even if the second line on the pregnancy test is barely noticeable, blurred and does not change color intensity for two or three days, then it is worth continuing to monitor the hCG level over time. To do this, you will need to do several tests or donate blood several times to check the hCG level, which will increase with a normally developing pregnancy or “tread water” with an ectopic form. With these incorrect tests, it is worth visiting a gynecologist.

With an ectopic pregnancy, the second stripe will not become brighter and clearer after a few days
Early diagnosis and treatment of non-uterine pregnancy will not only protect against removal of the organ housing the lost fetal cell, but will also prevent the woman from conceiving a child on her own in the future.
Knowing the accompanying signs, it will be easier to suspect an abnormal pregnancy, these are the distinctive points:
- cycle failure. “Pseudo-mentruation” occurs at the wrong time and lasts only a couple of days. Sometimes menstruation continues in the first month;
- brown discharge from the genital tract after the end of menstruation due to overstretching of the tube occupied by the fertilized egg and hemorrhages inside it;
- sharp, dagger-like or prolonged nagging attacks of pain in the lower abdomen, causing pain in the hypochondrium, anus, legs, sacrum for half an hour or several hours;
- signs of progressive internal bleeding:
- a sharp decrease in blood pressure, acceleration of the pulse, weak filling, up to loss of consciousness;
- pale skin with the appearance of beads of sweat on the forehead.
Based on a woman’s complaints, a gynecologist can suggest the location of improper attachment of the fertilized egg:
- if you experience pain on one side of the lower abdomen, which increases in intensity with fast walking, changing body position or physical activity, the fertilized egg is in the oviducts;
- if there is pain, the area of which can be indicated with one finger, moving to the lower back or towards the intestines, the passage of feces is very painful, and the attacks themselves are accompanied by fainting - ovarian pregnancy;
- if you are worried about a frequent urge to urinate and heavy bleeding without attacks of pain in the abdominal area - cervical or cervical-isthmus;
- if digestion is difficult due to vomiting, nausea, and the feces are denser or, conversely, too watery, and the attacks of pain are unbearable, then an abdominal variation of an ectopic pregnancy is suspected.
Video: obstetrician-gynecologist M. Borets about the symptoms of ectopic pregnancy
Diagnosis of ectopic pregnancy
Of course, the diagnosis is not made only on the basis of the doctor’s complaints and assumptions. Instrumental and laboratory techniques are used for confirmation.
- Self-diagnosis at home. To exclude ectopic pregnancy, from the fifth day of delay, it is recommended to repeat a pregnancy test over several days, which determines the level of hCG in the urine. Electronic types of tests are the most informative.

Such electronic tests not only detect hCG in urine, but also compare its measured level with norms for different stages of pregnancy
- Examination on the chair by a gynecologist. May reveal the following warning signs:
- pain on palpation of the appendages;
- the increased size of the appendages or pipes on one side is determined;
- the size of the uterus does not correlate with the duration of the expected pregnancy;
- the uterus is softer, but its size is smaller than expected.
- Laboratory test:
- analysis for the level of hCG or human chorionic gonadotropin, confirming the fact of pregnancy. It, as a rule, lags behind the normal level for several days or stops growing altogether in case of spontaneous miscarriage;
- analysis of progesterone levels, which will also be significantly lower than normal;
- a general blood test, which will determine inflammation in the organs by an increase in leukocytes and ESR, decreased levels of hemoglobin, red blood cells and hematocrit due to bleeding.
- Ultrasound examination of the pelvic organs, which can confirm or refute ectopic attachment, which has determined:

- Minimally invasive diagnostic laparoscopy, which allows you to make a definitively correct, undoubted diagnosis. With its help, the doctor examines the pelvic organs, determines the integrity of the tubes and the location of the development of the ectopic pregnancy.

This method is not traumatic; it will leave only 3 small scars 0.5–1.5 cm wide on the abdomen as a “memento” through which the instrument for internal examination and manipulation was inserted - tubes and a laparoscope
Thanks to minimally invasive diagnostic laparoscopy alone, the accuracy of diagnosing ectopic attachment of the fetal unit increased to 100%, while the combination of ultrasound with checking the hCG level gave a maximum of 95% probability, and with ultrasound alone - no more than 78%.
Medical care in the form of surgery or drug therapy
If the diagnosis of ectopic implantation is confirmed, the fertilized egg will be removed. Here, several options for further actions are possible, depending on the woman’s condition; the choice of the desired method remains with the doctor, who has all the collected data about the pregnancy. Only effective means Surgical methods are used to eliminate the ectopic form of pregnancy.
Since among all ectopic pregnancies, more than 90% of cases are tubal variations of egg arrest, surgical methods of intervention in the area of the fallopian tubes are the most studied and tested many times. In 40% of cases, after treatment of ectopic pregnancy, intrauterine pregnancy occurs.
Table: surgical methods for treating ectopic tubal pregnancy
After organ-conserving operations, after 2 days of postoperative recovery, it is necessary to monitor the level of hCG in the blood every 2 days, which ideally should be half the hCG value before surgery. If the hCG level has decreased by only 25%, then an additional intramuscular injection of methotrexate will be prescribed to stimulate the natural rejection of the trophoblast tissue remaining in the tube cavity after the operation.
Drug effects on ectopic pregnancy
It is possible to use a medical method of treating ectopic pregnancy without surgery if a number of conditions are met:
- Steadily developing ectopic pregnancy without bleeding;
- hCG level before treatment is less than 5000 mIU/ml;
- the size of the fertilized egg is no more than 2–3.5 cm;
- the embryo's heartbeat is not detected;
- The woman’s health condition allows the use of cytostatic drugs that block cell division and metabolism in them:
- the liver and kidneys work without failures;
- leukocytes in the blood are not reduced to 1.5 * 10 9 / l;
- platelets greater than 150*10 9 /l;
- short period of pregnancy, no more than 42 days of the non-menstrual period.
Photo gallery: drugs for terminating ectopic pregnancy
Mifegin is used once in the amount of 600 mg under the supervision of a doctor for 2 hours after taking Mefepristone is used once in a volume of 600 mg, always under the supervision of a doctor, sometimes in combination with misoprostol 400 mg to enhance the effect, and followed by ultrasound control after 1.5–2 days The drug for embryo rejection is administered intramuscularly, 1 injection every 2 days, and when the hCG decreases by 15%, the administration is stopped
Prediction of pregnancy development at various locations of the embryo and possible complications
The vast majority of types of ectopic pregnancy require immediate surgical intervention to remove the embryo that is developing in the wrong place and its membranes. Possible complications from a late detected ectopic pregnancy include:
- the development of internal bleeding with large blood losses, which lead to the development of hemorrhagic shock with the need to replace blood loss;
- rupture of the fallopian tube with the formation of scars inside the organ;
- loss of reproductive function. When removing an embryo from a sheltering organ during surgery, it may be necessary to remove the fetal sac (uterus, ovary, tube on one side) due to its overstretching or massive bleeding;
- hormonal imbalances from an interrupted pregnancy;
- the risk of repeating such an abnormal pregnancy after recovery;
- a fatal outcome when a woman loses not only the embryo, but also her life because inflammation in the organ has spread through the blood.
Table: type of ectopic pregnancy and possible outcome
Prevention of non-occurrence of ectopic pregnancy
No one is immune from such an abnormal pregnancy, but it is possible not to create the conditions that contribute to it.
- If a second fuzzy line is detected on the test, perform several home tests to confirm the increase in hCG levels.
- Prepare for pregnancy:
- take smears for infections transmitted from a sexual partner, especially for chlamydia and gonococci - the most ardent opponents of a normally developing pregnancy, causing an acute inflammatory process;
- undergo an ultrasound of the pelvic organs in order to find out whether the woman’s uterus is of the correct shape and whether there are signs of endometriosis or inflammation of the tissues of the internal organs;
- take blood tests to check the level of hormones, the lack or excess of which can direct the fertilized egg in the direction opposite to the uterus.
- Carefully treat old inflammations of the genitourinary system to prevent transmission of infection to the uterus.
- Use barrier contraception during pregnancy to prevent infection after conception;
- If you do not want to become a mother in the near future, choose a method of contraception that is suitable for you. You cannot take contraceptive pills that your friend takes, you cannot install an IUD without consulting a gynecologist and without an examination. For example, if a woman has a bicornuate uterus, installing an IUD is not at all effective, and even with a normal uterus shape it will not protect against ectopic pregnancy if barrier protection methods are not used.
- Be examined by a gynecologist as part of a medical examination at least once a year, if there are no complaints.
- Maintain careful hygiene of the genitals, wash the vaginal area after sexual intercourse, and during menstruation - after each urination. Morning and evening toileting of the vulva is mandatory.
- Quit smoking. Every year, the ability to bear children due to smoking decreases, and when the threshold of 10 years is reached, a woman enters a risk group with a high probability of developing an ectopic or ectopic pregnancy.
Video: gynecologist surgeon S. Novikov on the prevention of ectopic pregnancy
Doctors know what to do with such a pregnancy; each case has its own solution. But any delay in seeking medical help risks a woman losing her reproductive organs during surgery to remove an overgrown fertilized egg. To preserve fertility, it is worth monitoring the health of the pelvic organs and periodically visiting a gynecologist to undergo the necessary tests.
Signs of an ectopic pregnancy in the early stages are difficult to recognize and often go undetected. Early signs are similar to those of physiological pregnancy. Differences appear at a later date, from about 5–6 weeks.
Therefore, this condition often leads to the development of serious complications and unfavorable outcomes. In order to correctly and timely diagnose an ectopic pregnancy, it is necessary to know its types and early symptoms pathology.
What are the causes of ectopic pregnancy?
There are many factors that cause this pathology. These include:
- Inflammatory and purulent diseases of the reproductive organs.
They cause disturbances in the structure of the mucous membranes of the conductive tracts and a decrease in the contractility of muscle fibers in the tubes. As a result, the natural process of advancement of the fertilized egg into the uterine cavity is disrupted. And it lingers in the corresponding fallopian tube. Also, chronic inflammation can lead to blockage of the pipes, causing their obstruction.
- Anatomical features of the structure of the fallopian tubes.
They can be too long or tortuous, curved.
- Adhesions in the abdominal cavity after other surgical interventions. Adhesions also prevent the normal dislocation of the fertilized egg.
- Frequent and long-term use of contraceptives or use of an intrauterine device.
- Pathologies of the ovum. These include developmental anomalies, genetic disorders and the influence of external damaging factors.
- Often, an ectopic pregnancy develops in the early stages after in vitro fertilization.
- Infectious diseases of the reproductive system, especially those accompanied by high body temperature.
- Imbalance of hormones in the body.
- Frequent colds with fever.
- Hypothermia.
Types of ectopia and characteristic signs
There are 4 types of ectopia, which depend on the place of attachment of the fertilized egg:
This is the most common type, in which the fertilized egg is retained in the tube for some reason. Most often, the embryo develops in the ampulla of the tube. If this ectopia is not diagnosed in a timely manner, a rupture of the fallopian tube may occur. This occurs as a result of active growth of the embryo, starting from week 6.
This condition is an emergency and requires immediate hospitalization.
It manifests itself as severe abdominal pain, severe bleeding, a drop in blood pressure, and loss of consciousness. Moreover, the pain is typical on the side where ovulation supposedly took place and the fetus is developing. Dizziness and dry mucous membranes are noted. Body temperature may increase.

This option is less common and is associated with malformations of the uterus. If a woman knows about developmental pathology, then when the first symptoms of pregnancy appear, she must undergo ultrasound diagnostics immediately. It will help clarify the place of attachment of the embryo and decide on further tactics.
This is the most rare option, it is difficult to diagnose in time. With it, implantation of the fertilized egg occurs in the area of the internal organs of the abdomen. Signs of pregnancy in the early stages correspond to the normal course. The abdominal type is dangerous for a pregnant woman, as it leads to extensive bleeding in the abdominal cavity. If the fetus is sufficiently supplied with blood, then there is a chance to carry it to a viable term. But this rarely happens. Only isolated cases of the birth of viable children have been described.
With this type, 2 or more fetuses develop, one is located in the uterus, and the second is ectopic in an atypical place. At the same time, the increase in hCG and progesterone in the blood remains normal. Difficulties in diagnosis arise in unidentified multiple pregnancies. In the early stages, ultrasound detects one embryo in the uterus. This often leads to the condition being misdiagnosed.
The very first signs of ectopic embryo development
A fertilized egg can stop anywhere along the way from the ovary to the uterus. This may be the abdominal cavity, the ovarian area or the fallopian tube. This pathology occurs due to an inflammatory or adhesive process in the reproductive organs and abdominal cavity.

In this case, the very first symptoms of an ectopic pregnancy correspond to the early signs of uterine attachment of the embryo:
- there will be a delay in menstruation;
- the test will show a positive result in the form of two stripes;
- signs of toxicosis may appear;
- the mammary glands will become sensitive, slightly painful and enlarged;
- urination becomes more frequent;
- basal temperature will be elevated, as happens during physiological pregnancy; if the rectal temperature is below 37 degrees, then it is likely that the embryo has died;
- mood will become changeable;
- general body temperature can also rise to subfebrile values – 37.2–37.5 degrees.
What changes are typical for the test?
If you suspect you are pregnant, you can do a test at home. It should be done if there is a delay, fever and other signs. In case of an ectopic pregnancy, the test will show a positive result, but the test strip on it will not be bright enough. And after a couple of days the test may become negative.
If this is observed during testing, and characteristic symptoms are present, then you should immediately consult a doctor. In most cases, the diagnosis of ectopic pregnancy is confirmed. It is important to know that such signs can also occur during a physiological pregnancy that has stopped for some reason.

Symptoms of ectopic pregnancy in the first weeks
In addition to general signs in the early stages, ectopic pregnancy is characterized by specific symptoms:
- The appearance of bloody discharge from the genital tract similar to menstruation. They can be dark brown or brownish. It is important not to confuse them with menstruation if there has been a long delay. It must be remembered that there may not be visible bleeding if blood accumulates in the abdominal cavity.
- Along with the discharge, severe cutting pain appears in the abdominal area. In this case, the localization of pain depends on the part in which the embryo develops. The pain syndrome intensifies with movements and changes in body position.
- Characterized by general weakness, malaise, chills.
- Body temperature may rise. Basal temperature higher than general values, mostly low-grade.
- If there is large blood loss, dizziness and fainting occur. This reduces blood pressure.
What signs are found during the examination?
Ectopic pregnancy is detected in the early stages using the following examination:
- Blood test for hCG (human chorionic gonadotropin). This hormone begins to be produced early after implantation of the fertilized egg. If the embryo develops in the uterus, then hCG normally increases every 2 days. If its attachment occurs in an atypical place, then a slow growth of human chorionic gonadotropin is noted.
- A study of the level of progesterone in the blood is carried out. This is a hormone of the corpus luteum, which is responsible for maintaining pregnancy. With an ectopic pregnancy, progesterone levels will be low.
These 2 indicators are relative characteristics. They also change with non-developing intrauterine pregnancy or.
In addition, instrumental examination is carried out:
- Ultrasound examination of the pelvic organs.
It allows you to see the embryo in the early stages with hCG levels above 1500 IU/l from about 4-5 weeks. If the doctor does not see it in the uterine cavity by ultrasound, then the search continues in other areas: tubes, ovaries, abdominal cavity.

It is carried out when other methods fail to establish an accurate diagnosis. An audit of the pelvic organs is carried out. If a fertilized egg is detected in an atypical location, the pregnancy is terminated. Often, during surgery, the fallopian tube in which the pregnancy occurred is removed. It depends on the duration and accompanying complications.
Unfortunately, it is impossible to save the life of a developing fetus during an ectopic pregnancy. Therefore, therapeutic measures are aimed at preserving women’s health and her life. The critical period before which complications can be avoided is 6–8 weeks.
If unfavorable symptoms appear, accompanied by an increase in body temperature, you should immediately consult a doctor or call an ambulance. This is an emergency condition that requires qualified assistance. Late diagnosis and termination of such a pregnancy lead to serious complications or death.
 The bleeding in this case is not as pronounced as when a pipe ruptures. However, blood accumulating in the abdominal cavity contributes to the development of the inflammatory process, which is manifested by malaise and pain. In this case, the basal temperature during an ectopic pregnancy increases significantly and can reach 38 degrees.
The bleeding in this case is not as pronounced as when a pipe ruptures. However, blood accumulating in the abdominal cavity contributes to the development of the inflammatory process, which is manifested by malaise and pain. In this case, the basal temperature during an ectopic pregnancy increases significantly and can reach 38 degrees.